As we age, our bodies undergo significant changes, including in the urological system. Understanding these changes and addressing them proactively is key to maintaining a high quality of life. Urologists specialize in diagnosing and managing age-related urological conditions, helping individuals adapt to these transitions.
The Aging Urinary System
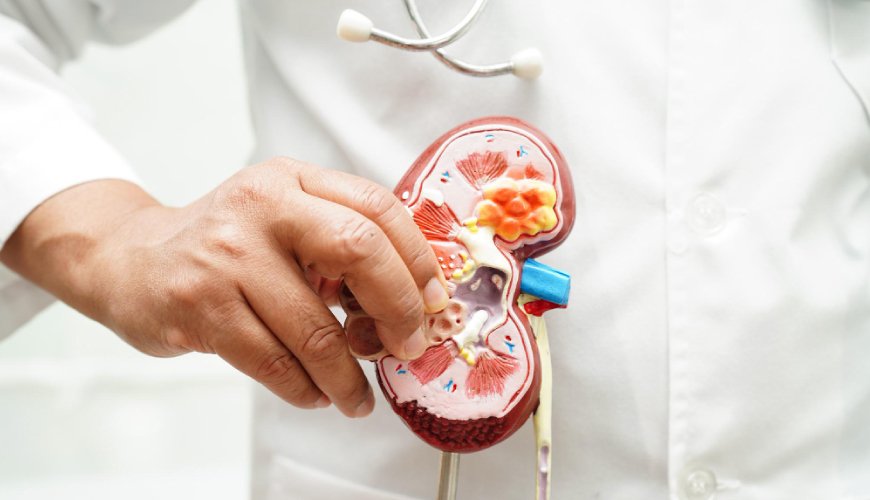
1. Reduced Kidney Function
- Natural Decline: Kidney function tends to decline with age due to reduced blood flow and the gradual loss of nephrons (kidney filtering units).
- Impact: This may lead to a decreased ability to filter waste and maintain fluid balance, increasing the risk of kidney disease.
2. Bladder Changes
- Weakened Bladder Muscles: Aging can reduce bladder elasticity and muscle strength, causing issues with urine storage and emptying.
- Overactive Bladder: A common condition where frequent urges to urinate disrupt daily life.
- Incontinence: Loss of bladder control may result from weakened muscles or nerve damage.
3. Prostate Enlargement (Men)
- Benign Prostatic Hyperplasia (BPH): Age-related prostate growth can cause urinary difficulties, such as a weak stream, frequent urination, or incomplete emptying.
4. Hormonal Changes
- Men: Declining testosterone levels can affect urinary and sexual function.
- Women: Post-menopause, reduced estrogen levels may lead to vaginal and urinary tract changes, increasing infection risk.
Common Age-Related Urological Conditions
1. Urinary Tract Infections (UTIs)
- Older adults, particularly women, are more prone to recurrent UTIs due to hormonal changes and weakened immune systems.
2. Kidney Stones
- Aging can increase the risk of kidney stones due to dehydration and dietary factors.
3. Pelvic Floor Disorders (Women)
- Conditions like pelvic organ prolapse and stress incontinence become more prevalent with age.
4. Erectile Dysfunction (Men)
- Affects many older men and is often linked to underlying health conditions like diabetes, heart disease, or hormonal imbalances.
Proactive Steps for Urological Health
1. Stay Hydrated
- Drink adequate water daily to support kidney function and prevent infections.
2. Maintain a Healthy Diet
- A balanced diet rich in fruits, vegetables, and low-sodium foods helps support overall urinary health.
3. Exercise Regularly
- Physical activity strengthens the pelvic floor muscles, aiding bladder control and reducing incontinence risks.
4. Routine Check-Ups
- Regular visits to a urologist can help detect and manage age-related conditions early.
5. Manage Chronic Conditions
- Control diabetes, hypertension, and other systemic illnesses to reduce their impact on the urinary system.
Treatment Options for Age-Related Conditions
1. Medications
- Urologists may prescribe drugs to manage overactive bladder, BPH, or erectile dysfunction.
2. Minimally Invasive Procedures
- Advanced techniques like laser therapy for BPH or laparoscopic surgery for kidney stones are effective with shorter recovery times.
3. Lifestyle Modifications
- Dietary changes, bladder training, and pelvic floor exercises can alleviate many urological symptoms.
4. Specialized Therapies for Women
- Vaginal estrogen therapy can address post-menopausal changes in urinary and vaginal health.
Conclusion
Aging brings inevitable changes, but with proactive care and regular consultations, you can manage your urological health effectively. By staying informed and addressing issues early, you can ensure a healthier, more comfortable aging process. Urologists are your partners in navigating these changes and preserving your quality of life.